Does Chemotherapy and Radiation Affect Tumor Necrosis in Soft Tissue Sarcoma?
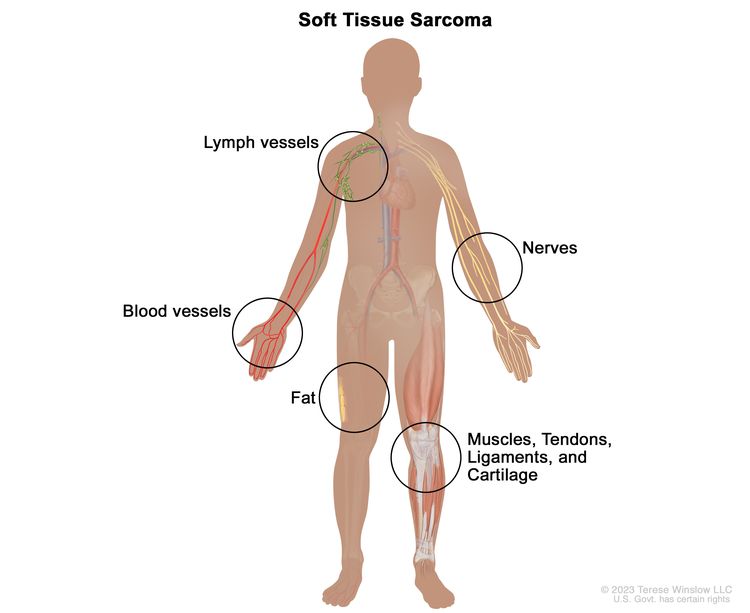
Soft tissue sarcomas (STS) are a rare and diverse group of tumors that can appear anywhere in the body. Treating STS usually involves surgery, often combined with chemotherapy or radiation therapy to shrink the tumor before removal. But does this pre-surgical treatment (called neoadjuvant therapy) really impact the tumor's necrosis (cell death), and does that affect survival?
Key Findings
Neoadjuvant Therapy Increases Tumor Necrosis
Patients who received chemotherapy and/or radiation had significantly higher tumor necrosis (53.5%) than those who did not (15.7%).
The combination of both therapies led to even greater necrosis compared to just radiation alone.
Necrosis Doesn't Predict Survival in STS
Unlike bone sarcomas, where necrosis is a strong predictor of survival, STS patients did not show a clear link between higher necrosis and better survival rates.
Other factors like tumor grade, size, and the presence of metastases were much stronger predictors of survival.
Surgical Margins Matter More for Local Recurrence
The completeness of tumor removal (R0 resection) played a more significant role in preventing local recurrence than tumor necrosis did.
What Does This Mean for STS Treatment?
While chemotherapy and radiation do increase tumor necrosis in STS, it doesn’t necessarily translate to better survival rates. Unlike in bone sarcomas, where necrosis is an important indicator of treatment success, STS outcomes are influenced more by tumor grade, size, and metastasis. This suggests that while neoadjuvant therapy is valuable, its effectiveness should not be judged solely by the amount of necrosis it induces.

