ACSL4's Role in Hepatoblastoma Progression and Therapeutic Targeting
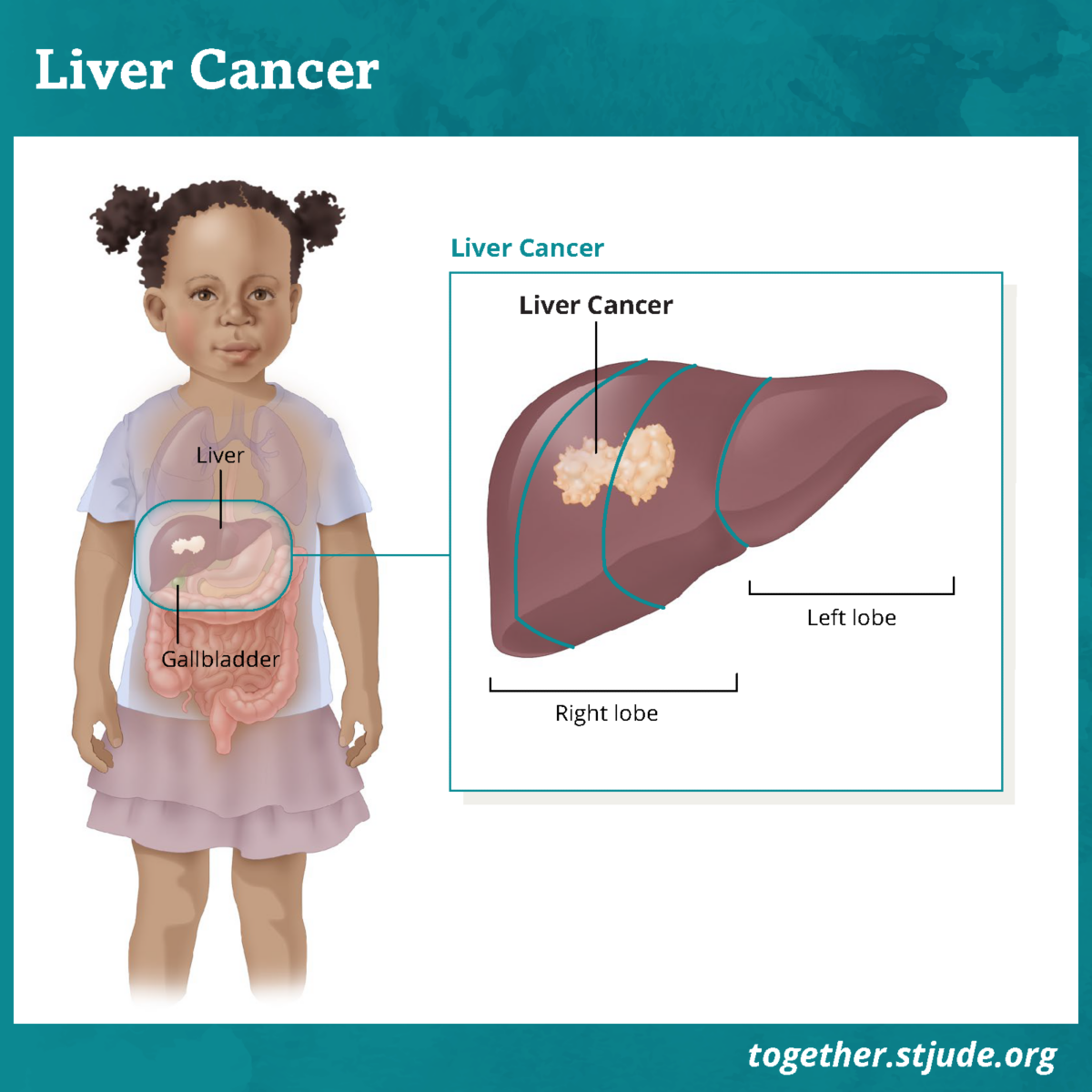
Hepatoblastoma is the most common liver cancer in children, with increasing incidence, particularly among those under five years old. Despite improvements in treatment, approximately 20% of cases remain resistant to chemotherapy or are deemed unresectable, leading to poor survival outcomes. Identifying high-risk patients and developing targeted therapies is crucial to improving prognosis.
Current clinical risk assessments rely heavily on imaging and histopathology, with serum alpha-fetoprotein being the only widely used molecular marker. However, hepatoblastoma is highly heterogeneous, making it difficult to classify patients based on conventional methods. Advances in genomic and transcriptomic analyses have led to the identification of molecular subtypes that can help refine risk prediction and treatment strategies.
How the Study Was Conducted
This study performed transcriptomic analysis on hepatoblastoma samples obtained from public gene expression databases. Clustering analysis identified three distinct molecular subtypes of hepatoblastoma, each with different prognostic outcomes. Among these, the proliferative subtype was characterized by a high proliferation rate, poor differentiation, and a highly immunosuppressive tumor microenvironment.
ACSL4, a key enzyme involved in fatty acid metabolism, emerged as a critical biomarker of the proliferative subtype. Researchers further explored its role in tumor progression through in vitro and in vivo experiments. Hepatoblastoma cell lines were genetically modified to knock down ACSL4 expression, and xenograft mouse models were used to study the effects of ACSL4 inhibition on tumor growth.
Key Findings on ACSL4 and Hepatoblastoma Progression
Patients classified under the proliferative subtype had significantly worse clinical outcomes compared to other subtypes. These tumors exhibited high expression of mitosis-related genes, including MKI67 and TOP2A, which are associated with aggressive tumor behavior.
ACSL4 was found to be highly expressed in the proliferative subtype, playing a central role in driving tumor growth. Knockdown of ACSL4 in hepatoblastoma cell lines led to a significant reduction in cell proliferation and colony formation. In xenograft models, pharmacological inhibition of ACSL4 using abemaciclib, a known ACSL4 inhibitor, effectively suppressed tumor growth.
Mechanistic studies revealed that ACSL4 promotes tumor progression by downregulating the interferon response signaling pathway. This suppression of immune signaling contributes to the immunosuppressive nature of the proliferative subtype, allowing tumor cells to evade immune detection.
The Immunosuppressive Microenvironment of the Proliferative Subtype
Further analysis of the tumor microenvironment showed that the proliferative subtype had reduced immune infiltration. Levels of key immune cells, including macrophages, dendritic cells, and memory B cells, were significantly lower in this subtype. Additionally, inflammatory and immune response-related genes such as IL-18, IL-6, and TNF were downregulated.
This suggests that ACSL4 not only drives tumor proliferation but also contributes to immune evasion. By inhibiting interferon signaling, ACSL4 helps maintain a tumor environment that is resistant to immune-mediated destruction.
Given its role in promoting tumor growth and immune evasion, ACSL4 represents a promising therapeutic target for hepatoblastoma. This study demonstrated that targeting ACSL4 with abemaciclib led to significant tumor growth suppression in preclinical models.
Abemaciclib is already approved for use in other cancers, particularly breast cancer, where it functions as a CDK4/6 inhibitor. However, recent studies have shown that it also binds to ACSL4, making it a potential candidate for hepatoblastoma treatment.
To learn more, read this!: ACSL4 promotes the formation of the proliferative subtype in hepatoblastoma | BMC Cancer | Full Text